Women's Hormone Health Linked To Productivity Working With Peri-/Menopause
Thursday 10 October 2024
.jpg?width=493&height=350&ext=.jpg)
By Katherine Kelly (AfN, mBANT), Founder & Nutritionist at Renua Nutrition.
You are not alone in thinking that your work life is being impacted by peri-/menopausal symptoms. A study on women in Healthcare showed that 65% of women over 50 years were seeing their work being affected by these symptoms and 18% had to take sick leave (O’Neill, et al). This article explores what is happening in our bodies during this phase of life, how our work lives are affected and finally gives nutrition and lifestyle interventions that can help.
What Is The Perimenopause?
The perimenopause is the stage before the menopause (one year without a period). It typically starts two to ten years before the final period. You might start to notice a change in your cycle, for example a change in length or flow.
Symptoms occur mostly during perimenopause and are temporary however they can be debilitating and make daily tasks more challenging.
The most common symptoms experienced are:
- Mood & sleep disturbances
- Hot flashes and night sweats
- Heart palpitations
- Migraines
- Heavier periods
- Breast pain
- Vaginal dryness
- Abdominal weight
- Body aches and pains
*These symptoms can also be caused by other medical conditions so do check with your GP if you are experiencing any of them.
The final period is typically from 45 to 55 yrs - and the average time of the perimenopause is 7 years. This does not mean you will have symptoms for 7 years as individuals can go through this stage of life noticing no symptoms at all.
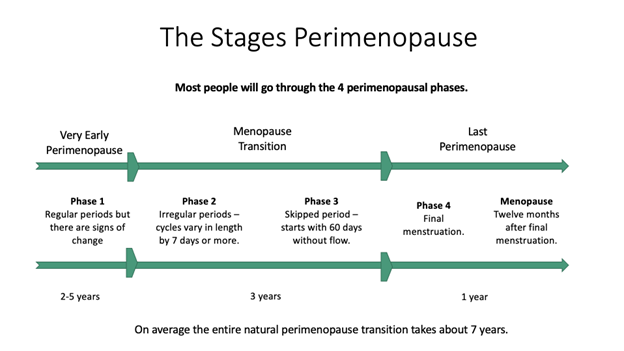
Figure 1: The four phases perimenopause. Adapted from: Laura Briden, hormone repair manual, Greenpeak publishing, 2021
What Exactly Happens To Our Hormones During Perimenopause?
The first stage of the perimenopause is losing progesterone which typically starts in your 40’s but can occur in late 30’s. Losing progesterone when you still have lots of oestrogen is the cause of many perimenopausal symptoms including: migraines, anxiety, heart palpitations, breast pain, heavy periods. The last time we experienced this hormonal shift was during puberty, so if some of your symptoms feel the same this could be why.
Whilst this is occuring you may have up to 3 times higher oestrogen levels than you are used to experiencing and this can lead to irritability, heavy periods and breast pain.
After your final period oestrogen levels will decrease and you will enter the next phase of life - the menopause. Many of the menopausal symptoms come from this drop from high to low oestrogen. This can result in insomnia, memory loss, vaginal dryness, and weight gain.
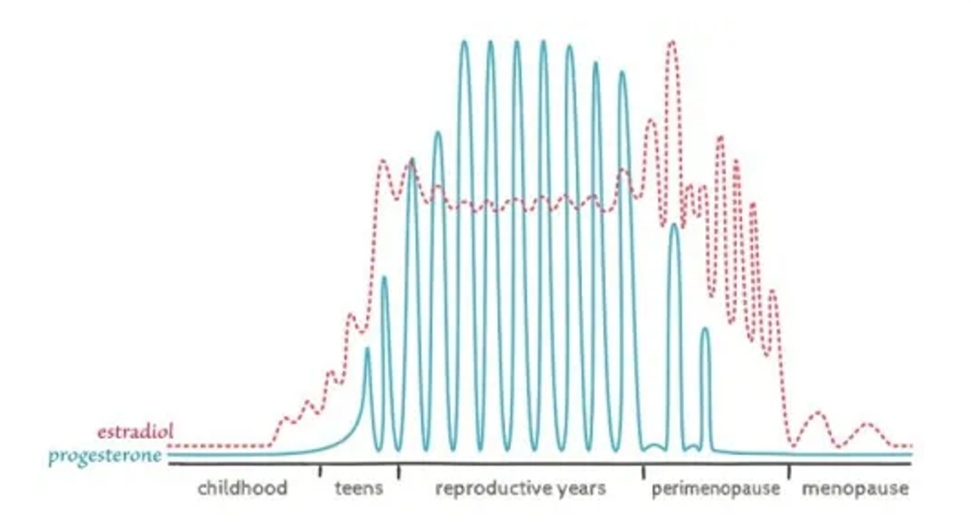
Figure 2: Hormones through the lifespan, adapted from JC prior, “Perimenopause lost - reframing the end of menstruation.”
How This Impacts Our Productivity
With the menopause being discussed more in the media and women in their 50’s being one of the fastest growing employment groups, this is a key area of healthcare. Research being done on this stage of life highlights the impact it is having on women’s careers. We now have work related cross sectional studies that support the knowledge that we have on menopausal symptoms, stating that these symptoms affect women’s quality of life, productivity at work, attendance at work and career decisions (Evandrou, et al., 2021; O’Neil, et al,. 2023 Whiteley, et al., 2013). The symptoms that most significantly impacted women's performance and attendance at work include: fatigue, difficulties sleeping, poor concentration, and poor memory.
The best work intervention was found to be manager awareness and flexible work schedules.
Nutritional & Lifestyle Interventions That Can Help
Practice Good Sleep Hygiene
- Go to bed at the same time every night and get up at the same time every day - even at the weekend - this keeps your circadian rhythm happy.
- Get 10-15 mins sunlight exposure (don’t wear sunglasses) first thing in the morning. This helps reset your circadian rhythm.
- Wind down 2 hours before bed - this means not doing anything too stimulating. Avoid watching TV in the last hour before your bedtime. Create a self-care routine for yourself: bath, skincare, meditation, reading etc…
- Maintain a cool and dark bedroom. 18 degrees celsius is the optimal temperature.
- Avoid eating in the last 2 hrs before bed.
- Stop consuming caffeine after 3pm.
- Take an epsom salt bath 1.5-2 hrs before bed - this give your body temperature time to cool down after the bath.
- Herbal tea - you can have this before bed as it doesn't contain any calories. Choose one that helps promote sleep eg. chamomile / Pukka nighttime tea.
Movement
Any kind of exercise can improve cognitive function, so this can be as simple as walking everyday. Yoga has good evidence to support the reduction of psychological symptoms during the perimenopause (Cramer et la,. 2012). This includes improvements in mood, anxiety, low self-esteem and brain fog. Building muscle mass is also important during this phase of life as it helps protect against Sarcopenia and helps reduce risk of osteoporosis (Briden, 2021). You can use your own body weight for example doing lunges, squats and planks or use additional weights. Ideally you want to do resistance training 3 days a week to see an improvement in your muscle mass.
Dietary Interventions
Insulin resistance can occur at this stage of life with the drop in oestrogen. This means your body can’t reduce its levels of glucose as well as it used to and this can also lead to weight gain. You may notice that higher sugar foods cause issue with mood irritability and concentration. To manage this you want to monitor your carbohydrate intake more carefully than you may have done in your younger years.
- Reduce white refined carbohydrates - this includes: white bread, pasta and rice. It also includes processed foods like: biscuits, cakes, cereal bars, low fibre cereals.
- Reduce intake of high sugar foods eg. fizzy drinks, sweets, milk chocolate.
- Increase your fibre intake - add extra vegetables to your meals, always choose wholegrain carbohydrates (bread, rice, pasta), consume nuts, seeds, lentils, chickpeas and beans.
- Eat protein with every meal. This includes both animal sources and vegetarian sources (tofu, lentils, chickpeas, beans, quinoa).
- Reduce alcohol - which can cause spikes in blood glucose due to the high sugar content.
Written by: Katherine Kelly | Registered Nutritionist & Nutritional Therapist (Afn, mBANT). Renua Nutrition.
References
Cramer H, Lauche R, Langhorst J, Dobos G. Effectiveness of yoga for menopausal symptoms: a systematic review and meta-analysis of randomized controlled trials. Evid Based Complement Alternat Med. 2012;2012:863905. doi: 10.1155/2012/863905. Epub 2012 Nov 7. PMID: 23304220; PMCID: PMC3524799.
Briden L, Hormone Repair Manual, Greenpeak publishing, 2021
Evandrou, M., Falkingham, J., Qin, M. and Vlachantoni, A., 2021. Menopausal transition and change in employment: Evidence from the National Child Development Study. Maturitas, 143, pp.96-104.
O'Neill MT, Jones V, Reid A. Impact of menopausal symptoms on work and careers: a cross-sectional study. Occup Med (Lond). 2023 Sep 29;73(6):332-338. doi: 10.1093/occmed/kqad078. PMID: 37542726; PMCID: PMC10540666.
Whiteley, J., DiBonaventura, M.D., Wagner, J.S., Alvir, J. and Shah, S., 2013. The impact of menopausal symptoms on quality of life, productivity, and economic outcomes. Journal of women’s health, 22(11), pp.983-990.
Thursday 10 October 2024


 Contact us
Contact us
 Share on social
Share on social Share with a friend
Share with a friend Facebook
Facebook LinkedIn
LinkedIn
 Twitter
Twitter




















 Get in touch with us
Get in touch with us